Lighting a Candle
America faces a shortage of health care professionals across the board. Nowhere is the problem more pronounced than in the rural south. Brenau nursing practice graduate Myron Faircloth is doing something about it.
THE ASSOCIATION OF AMERICAN MEDICAL COLLEGES estimates that by 2020, there will be a shortage of 45,000 primary care physicians with demand far outstripping supply. The shortage will affect the United States across the board, but it will have its greatest impacts on those communities that already suffer from shortages.
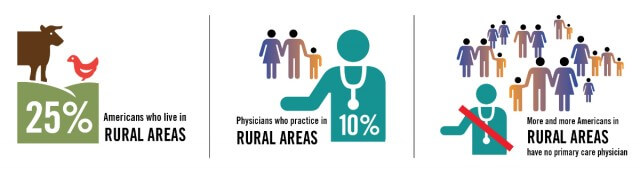
For example, 25 percent of Americans live in rural areas. By contrast, only about 10 percent of physicians practice in those places. “Fifty years ago, half of the doctors in America practiced primary care, but today fewer than one in three do,” the U.S. Senate Primary Health and Aging subcommittee reported in January. Fewer than 10 percent of the 17,000 new doctors graduating from medical school each year choose primary care careers. More and more Americans, especially in rural areas, say they have no primary care doctor. According to a study of the uninsured produced by graduate students in the health and medical journalism program at the University of Georgia, the situation will get worse before it gets better.
Here’s A Solution
Perhaps the best way to understand rural health care in Georgia – and the possible solutions to the scarcity of health care services in rural areas – is to look at J. Myron Faircloth, BU ’02, and his South Georgia hometown, Morven.

When Faircloth was 10, his family moved from Atlanta to Morven, which is located in Brooks County just north of Georgia’s southern border with Florida and west of Valdosta. His mother, Pat, a registered nurse, worked at Smith Hospital in Hahira, located a 15-minute drive away on the I-75 corridor.
During Faircloth’s boyhood days, rules were a little looser. He hung around with his mother at work, even visiting patients and getting to know them. He liked that. However, it is where he first learned how hard nursing could be.
“Her biggest disappointment was when she would lose a patient, but I saw my mother just give and give and give and just love that field,” said Faircloth. “That’s probably the biggest influence I had.”
Following her example, Faircloth earned a Bachelor of Science in Nursing degree at Valdosta State University. He worked in emergency rooms in the area and eventually wound up at South Georgia Medical Center about six blocks away from the campus. By then, he had forsworn his undergraduate oath never to return to the classroom.
“I think you get those influences from people you work with. You work alongside physician assistants, nurse practitioners, physicians,” he explained. “You see the role in how they help people, and you see that you want to further your education. I figured I could do more for my hometown that way.”
Faircloth, who now lives in Hahira and teaches at Valdosta State, enrolled in a graduate nursing program at Brenau University in Gainesville. He worked three 12-hour shifts during the week at SGMC, then drove 280 miles up on Thursdays, went to class for five hours straight, and then make the four-and-a-half hour trek back home. His goal was to become a family nurse practitioner.
Similar to physician assistants, nurse practitioners have earned master’s degrees or doctorates in nursing specialties like family practice, pediatrics or women’s health. Duties NPs perform vary by state, but generally include diagnosing and treating illness or injury, prescribing medication and other care management tasks. In Georgia, an NP working under the supervision of a medical doctor may make diagnoses and treatment recommendations but cannot prescribe drugs without the supervising physician’s approval.
Brenau’s strategic plan addresses the shortage of health care professionals, and the ForeverGold campaign places major emphasis on funding development and growth of those professional programs. The three Brenau doctoral programs all aim at reducing the growing load on primary care physicians through production of people skilled in preventive, therapeutic and rehabilitative arts.
The university also offers a physician assistant master’s degree-level program through a partnership with Philadelphia College of Osteopathic Medicine. However, according to Brenau College of Health Sciences Dean Gale Starich, the shortage of professionals is so acute that the university may also develop its own PA program.
Expanding Skills
After Faircloth finished a Master of Science in nursing at Brenau, he grew more drawn to rural, general practice work. The Brenau degree, he said, taught him, among other things, that in a rural setting where you are essentially the primary care provider, you have to be on your toes and wear all kinds of hats.
 “In the country, where you can be the only practitioner out there, you’ve got to be able to see patients across the lifespan, from pediatrics to adults,” he said. “That’s the most rewarding part of rural practice. You might treat teenagers, adults, infants or children. You have to stay on your toes. It’s not just a one type of patient population. I get to see it all.”
“In the country, where you can be the only practitioner out there, you’ve got to be able to see patients across the lifespan, from pediatrics to adults,” he said. “That’s the most rewarding part of rural practice. You might treat teenagers, adults, infants or children. You have to stay on your toes. It’s not just a one type of patient population. I get to see it all.”
For him, at least, that meant he had to broaden his own horizons beyond the doors of the hospital emergency room or rural clinic. He has to be able to find ways to meet patients’ needs other than taking temperatures, diagnosing an illness and prescribing treatment. Meeting needs, he discovered, includes doing things in addition to health care.
As he began his teaching career at Valdosta State, he enrolled in its nursing practice doctoral program. One class he took involved grant writing, a how-to course in shaking the money tree in government agencies, corporations and non-profit organizations for specific purposes. He focused on writing grant applications for the working uninsured and in rural family medicine. That’s where he got into health care policy, looking at the legislative side of his lifelong passion.
He also put on a lobbyist hat, working with the Georgia legislature on a bill to extended new permissions to nurse practitioners and physician’s assistants. That led to his appointment to the special Georgia advisory Commission on Mandated Health Insurance. The commission looks at proposed legislation and determines the financial and social impacts of it, as well as the feasibility if enacted.
Faircloth’s mom was a major influence, and so was his hometown.Because of his inherent love for small towns, especially his own, when Morven town leaders approached him about opening up a clinic there, he went all in.
“You always want to give back to your community. That’s one of the greatest things you can do.” he said, “But the problem in the rural areas is you have people who, A, don’t have insurance, or B, they don’t have transportation, or C, they don’t have the money and the time to go [to the doctor]. The major thing they don’t have, though, is access to is a provider.”
For hourly workers, taking time off is money lost, on top of the cost of transportation, medication and the doctor visit itself.
“They ask themselves, what’s more important: staying at work and feeding my family or this little bit of high blood pressure I’ve been dealing with? So, they tend to neglect health care,” Faircloth said. “But you don’t need to wait 40 years to deal with high blood pressure. You need to get it early on so you can decrease mortality and morbidity. It can lead to kidney disease. How do you prevent that? Treat it early on.”
Community Buy-In
The problem with opening a clinic in Morven is that, like most rural towns, Morven is small.
How small? Peach trees in Morven outnumber its 550 citizens. To be fair, Morven is known for its peach trees. Still, Morven has no stoplight, just a blinking caution light where the main roads intersect. Running a clinic is not cheap. Most people don’t want to build a clinic in an area where there aren’t many potential clients.
Morven and Faircloth have found a way around that. Peach City Walk-In Clinic is a true community clinic. It operates in the town’s old post office. Building owners Dan and Jackie McCloud – who also run the town’s stellar seafood restaurant, Pike’s Landing – offered him use of the building free of charge.
“I am most humbled, most honored, most grateful to have that,” Faircloth said. “It’s good to see they want to see success here; they want to have a provider.”
The building was an empty shell, but Faircloth acquired some sheetrock and, along with some volunteers, put up walls and installed a shower and a second bathroom with supplies he got from a local Habitat for Humanity store. Coombs, a local heating and air business, donated an air conditioning unit. One of the local churches, Morrison Baptist, held a drive for supplies: bandages, gauze, alcohol, peroxide.
City officials walked him through all the red tape that comes with opening a clinic: securing a business license, getting the power turned on and other routine headaches.
Faircloth runs the clinic along with Drs. Vera and Alberto Garcia, proprietors of G & C Family Medicine, the practice in Valdosta and Hahira where Faircloth has his “day job.”
Essentially, Peach City removes all the excuses someone could have for not going to the doctor. No transportation? It’s right in the middle of town, a couple of blocks from the town grocery store. Can’t take time off work? It is open evenings and weekends. Don’t have insurance? The clinic does not take insurance, just a flat fee for service.
When Peach Tree Walk-In Clinic first received patients, it was open only three days a week, but now the clinic has expanded to five: Tuesday, Thursday and Friday evenings as well as weekends.
The clinic averaged 10 to 15 patients per week in summer, the slowest time of the year, when the usual patient complaints are swimmer’s ear, sunburn, poison ivy, random accidents and other summer problems. When the fall weather kicked in, kids went back to school, and business picked up.
“Seeing 10 to 15 people a week last summer, if I had been responsible for overhead, rent, I could not have paid that,” said Faircloth. “That’s what the joy of this place is. I would not have been able to open this place up without the donations.”
Promoting Health
There is another thing you need to know about Faircloth: He is kind of a promoter. If there is a member of Congress, legislator or other public official near the place, Faircloth has a knack for getting him or her to the clinic for photo ops, followed by a story in the newspaper. He’s always thinking, too, about other ways to promote the facility to remind people that it is available to them. For example, he wants to host a health fair at the clinic, using students to check blood pressure and cholesterol levels. He plans to bring in other students studying athletic training, sports medicine, communication disorders, family counseling and other specialties to extend clinic services while offering students a place to train, practice and develop their skills.

In addition, he is spreading his influence locally. The most recent example is that on Dec. 17, 2014, nurse practitioner/clinic operator/ entrepreneur J. Myron Faircloth graduated from Abraham Baldwin Agricultural College in Tifton, Georgia, with another undergraduate degree – this one in criminal justice. “While I am practicing medicine at my clinic in Morven,” he said, “I will also be the new patrol officer on the city police force.”
All of Faircloth’s work converges. His work at G & C informs his teaching. The research he does for lesson planning informs his work at the clinic. The students he teaches can practice at the clinic and perhaps take that experience back to their own towns.
“I have the best of all worlds, I really do,” he said. “I get to come out here, see patients, and then drive three miles up the road to get the best home-cooked meal from my mom. I don’t know what else I could ask for.”
Rural clinics like Peach City also can serve as bases for specialists, giving podiatrists, dermatologists, cardiologists, physical therapists, occupational therapists and others a facility to visit and from which to operate.
“If you get patients involved with their health care and educate them, you’ll empower them. They’ll do much, much better with diet, exercise, if you just empower them,” he said.
What’s next for Faircloth?
“Who knows? It’s like anything else. Maybe you mentor a student and become an inspiration to that student,” he said. “Maybe they go back to their small little town and do this. Maybe they decide to come out here and help me. I would welcome that.”
Stuart Taylor is a freelance writer in Valdosta, Georgia.